From telehealth updates to GME requirements, here’s what you need to know, along with expert tips on making the process as easy as possible.
July 14, 2021 WednesdayFor many physicians, getting a medical license is the fulfillment of a lifetime dream. After years of hard work, the ability to practice independently is finally within reach.
Medical licensure is required of anyone who wants to practice medicine in the United States. But the process is complex, different in each state, and always evolving.
The following are basic requirements for medical licensure—including some things that have changed in recent years—and tips for making the process easier.
Before gaining a medical license, a physician must complete certain requirements. These include:
Applicants must submit proof of these accomplishments and also provide details about their work history. They also must reveal any information that may impact their ability to practice, including malpractice judgments and settlements or criminal convictions.
During the licensure application process, you likely will be asked questions about your personal history and background, notes Joe Knickrehm, vice president of communications for the Federation of State Medical Boards (FSMB).
This includes your work history and any physical and mental conditions that might impact your ability to practice medicine effectively. In many states, a criminal background check also will be part of the process.
“Those who meet a state or territory’s qualifications are granted permission to practice medicine in that state,” Knickrehm says.
Some doctors also pursue board certification, which requires physicians to complete specialty examinations that go beyond a state’s minimum licensure requirements.
The FSMB offers a series of free, online education modules that explain the licensure process, Knickrehm says. The FSMB also offers a page explaining in detail the process of becoming licensed by a state medical board. The AOA tracks each state’s licensure requirements, including GME, in its U.S. Licensure Summary (PDF; login required), which is free for AOA members.
Once basic requirements have been satisfied, the physician can apply for a medical license, or multiple licenses if the doctor plans to offer clinical medical services in more than one state.
When you apply for a medical license, expect both your education and graduate training to be verified. Although the exact rules vary from state to state, the application process itself and the information requested of you typically is similar wherever you plan to practice.
As part of your application process, you will be expected to provide:
Keep this information at hand and make copies of any completed materials. This might help if you apply for licensure in another state in the future.
One of the most common mistakes in the licensure process is failing to submit all necessary documentation, says Raine Richards, AOA director of state government affairs.
Boards face a large volume of applications, Richards says. “Many boards will not respond to inquiries regarding application status unless the physician has already submitted all required documentation,” she says.
Candidates often fail to allow adequate time for processing, she adds. “It can take six months or more for application processing in some states,” Richards says.
Richards urges candidates to, whenever possible, apply for licensure well in advance of applying for—or accepting—a job. In many states, osteopathic physicians are eligible to apply for licensure as early as their second year of postgraduate training, provided that they have completed a full licensing exam series.
While the journey to full licensure can be time-consuming and arduous, there are things you can do to make the process easier.
Richards suggests reviewing the requirements and deadlines in states where you are considering applying for licensure, and doing so as early as possible—certainly before accepting a job offer in one of those states.
She notes that some states require postgraduate trainees to obtain a temporary license, while others do not. In addition, while many states require just one year of postgraduate training before allowing physicians to obtain full medical licensure, some do require 24 or even 36 months of GME.
Further, some states require osteopathic physicians to complete the full COMLEX-USA examination series for licensure, and do not accept the USMLE. See your state’s GME requirements here (PDF; AOA login required).
“It is important to research the requirements in any state that you may be considering,” Richards says.
One way to streamline the licensure process is to use AOA Profiles. An osteopathic physician can use this service to help state licensing boards verify their credentials, says Maura Biszewski, AOA vice president of graduate medical education.
An AOA Profile includes primary source information about your:
Using this service allows you to have your medical school transcripts, board scores and residency information sent to state licensing boards. The service is free for AOA members and $25 for non-members.
“My biggest tip would be to ensure that your AOA Profile is up to date,” Biszewski says.
Once you get your license, you usually will need to renew it every year or two, depending on your state’s laws. To earn renewal, you will need to show that you have kept acceptable standards of ethics and medical practice. In most states, you also will need to show that you have participated in a continuing medical education program.
As with so many things in life, the rules for getting a medical license are constantly changing. One of the biggest recent shifts occurred in 2019, when California became the first state to require all DOs and MDs to finish 36 months of graduate medical education before becoming eligible for a full medical license.
The change in California arrived in the wake of the FSMB’s recommendation that boards require 36 months of GME for full licensure.
In some states, just a year of GME is required, though rules vary from state to state. Alaska and Connecticut each require at least 24 months of accredited GME before licensure.
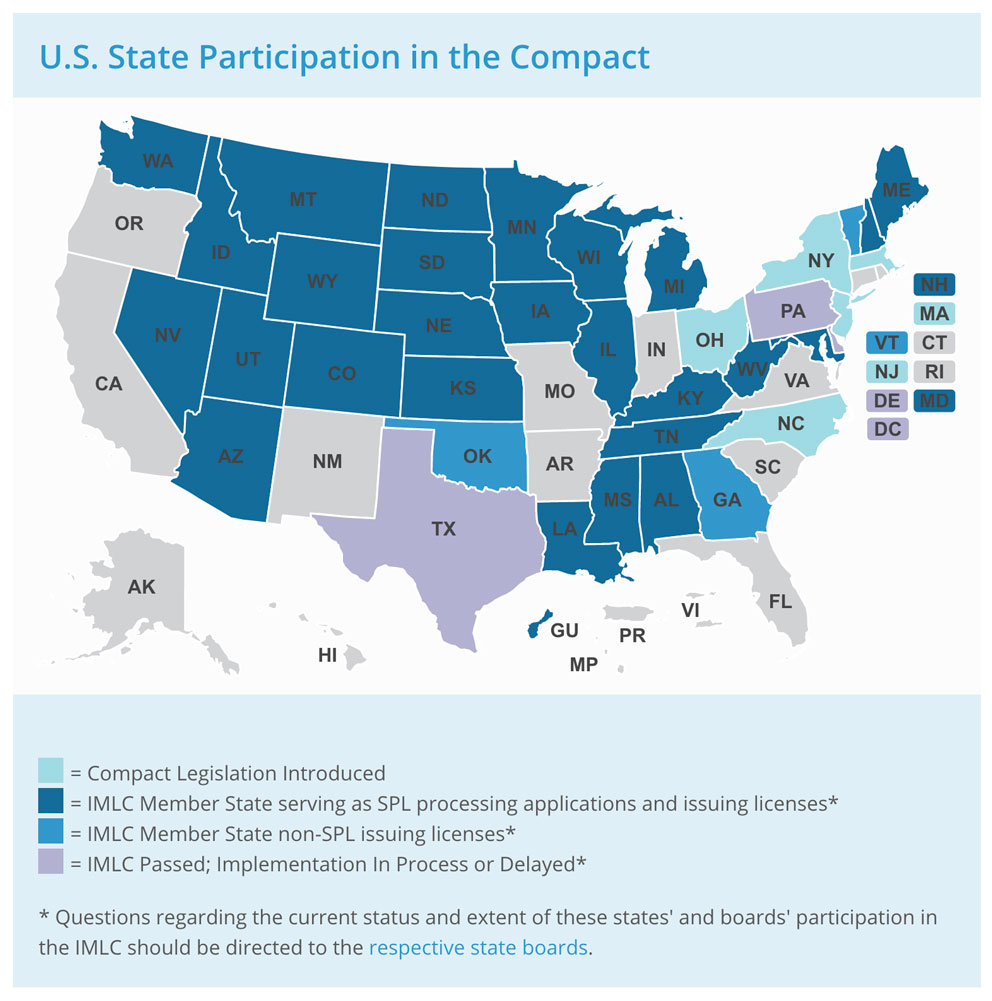
Another big change centers on the growing role of the Interstate Medical Licensure Compact (IMLC), which offers physicians an expedited pathway for becoming licensed in multiple states. Physicians can qualify to practice medicine across state lines within the compact if they meet its eligibility requirements.
“Roughly 80% of U.S. physicians meet the compact’s eligibility requirements,” Knickrehm says.
One of the eligibility requirements is that a physician must already have a full, unrestricted medical license from one of the states that is in the compact and is eligible to serve as the state of principal license (SPL).
Eligible physicians can complete just one application, which is reviewed by their SPL, and if the physician meets all requirements, the SPL issues a letter of qualification. The physician then selects the states in which s/he wishes to be licensed, and upon receiving their letter of qualification, each chosen state issues a license.
This expedites the overall licensure process, but physicians should know that after issuing a license to a physician who has received a letter of qualification, the medical board that has issued the license may ask for additional, ancillary information to fulfill the requirements of their respective medical practice act and their operational requirements. The license holder is required to comply with these requests, and failure to do so may result in action against the license by the issuing medical board.
Since 2017, 32 states, the District of Columbia and the U.S. island territory of Guam have all passed legislation to enact the compact in their jurisdictions. More states are considering joining, Knickrehm says.
One thing to keep in mind is that physicians using the compact will still have to pay separate licensure fees for each state. The IMLC maintains a list of state licensure fees here.
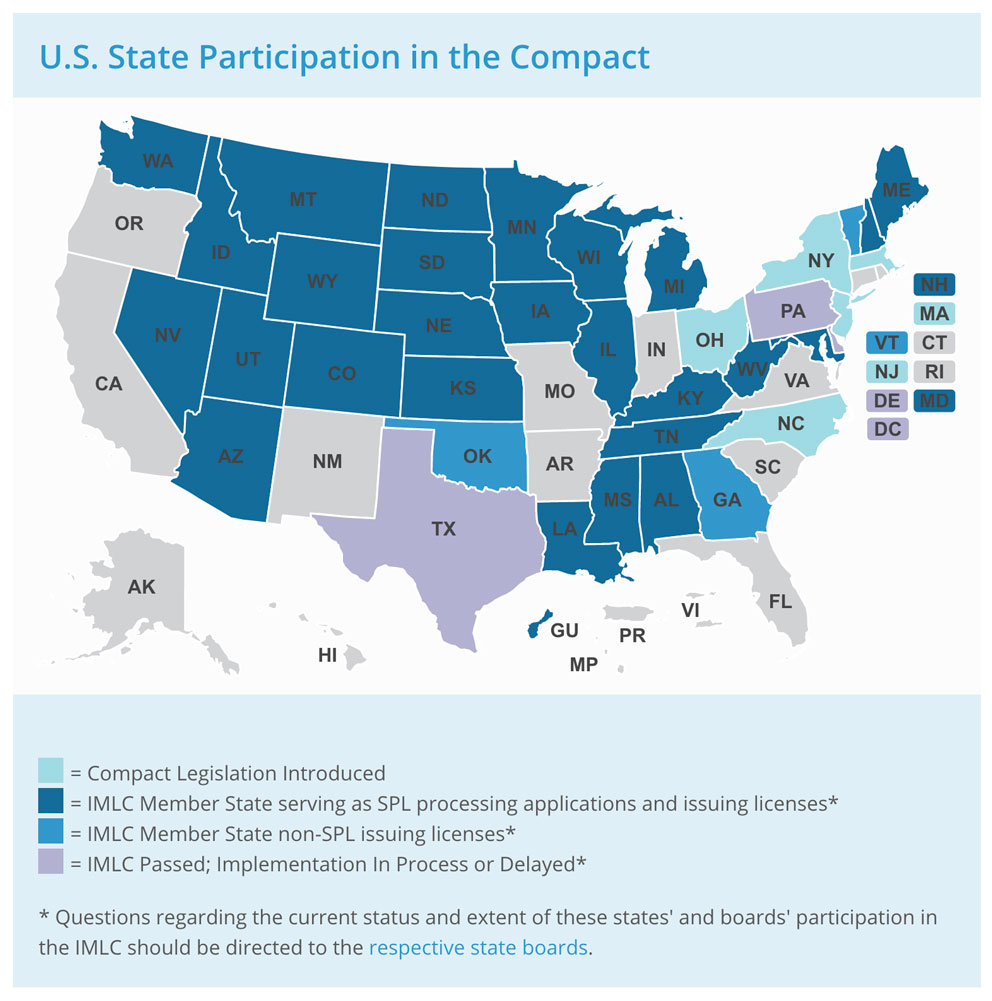
“More than 20,000 medical licenses have been issued using the compact process,” Knickrehm says.
Finally, as the role of telemedicine has grown, it has sparked questions about licensure requirements for remote medical care. About a dozen states issue licenses specific to telemedicine within their borders, Knickrehm says.
Florida, for example, recently established an “Out-of-State Telehealth Provider Registration,” which allows licensed out-of-state physicians to register to provide telehealth to Florida patients without obtaining a Florida license.
However, a full and unrestricted license to practice medicine in any jurisdiction in the United States typically covers both in-person care and telemedicine within that jurisdiction, he notes.
“You will not usually need a special license to practice telemedicine in a state where you obtain licensure,” Knickrehm says.